Myelodysplastic Syndromes (MDS): Quick Guide for Patients
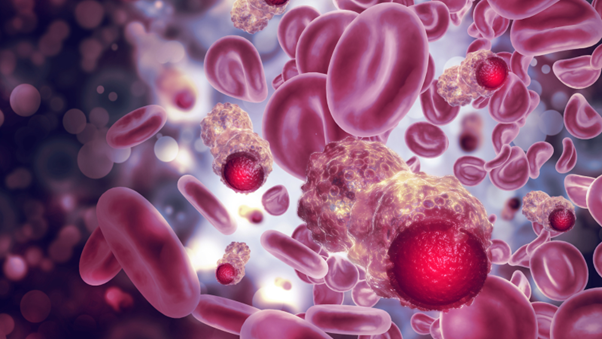
Myelodysplastic syndromes (MDS) are a group of blood cancers that affect the bone marrow and blood cell production. They are sometimes called bone marrow failure disorders and have a variable course.
When left untreated, MDS can lead to severe anemia, recurrent infections, uncontrolled bleeding, and in many cases progress to acute myeloid leukemia (AML), an aggressive form of blood cancer.
Because symptoms may appear gradually and resemble other conditions, MDS is often diagnosed late. Early detection and treatment are crucial to improve quality of life, prevent complications, and increase the chances of slowing or stopping disease progression.
What Are Myelodysplastic Syndromes?
MDS are clonal disorders of hematopoietic stem cells, meaning that abnormal stem cells in the bone marrow multiply and fail to produce healthy blood cells. This leads to:
- Dysplasia: abnormal cell structure
- Hyperplasia: excessive bone marrow growth
- Cytopenia: low levels of red blood cells, white blood cells, or platelets
MDS can be classified into two main types:
- Primary MDS – no identifiable cause (most cases)
- Secondary MDS – develops after chemotherapy, radiation therapy, or exposure to toxic substances
Causes and Risk Factors
The exact cause of primary MDS is unknown. However, several risk factors increase the likelihood of developing the disease:
- Long-term exposure to chemicals such as benzene, toluene, xylene, and herbicides
- Tobacco smoke
- Excessive alcohol use
- Contact with heavy metals
- History of aplastic anemia
- Prior chemotherapy or radiotherapy (for secondary MDS)
Age is the strongest risk factor, as most patients are diagnosed at 70 years or older.
Symptoms of MDS
Many patients with MDS have no symptoms at first and are diagnosed during routine blood tests. When symptoms appear, they are often related to cytopenias:
- Anemia (low red blood cells): fatigue, weakness, pale skin, shortness of breath
- Neutropenia (low white blood cells): recurrent infections, fever
- Thrombocytopenia (low platelets): easy bruising, frequent nosebleeds, prolonged bleeding
Diagnosis of MDS
Because MDS symptoms overlap with other conditions, an accurate diagnosis requires a detailed evaluation. Doctors will review:
- Medical history: medications, alcohol/tobacco use, prior cancer treatments, occupational exposures
- Physical examination and blood tests
- Bone marrow biopsy
Minimum Diagnostic Criteria for MDS:
- Persistent cytopenia in at least one blood cell lineage for more than 6 months
- Dysplasia in ≥10% of cells in at least one lineage
- Cytogenetic abnormalities typical of MDS
- 5–19% myeloblasts in bone marrow
A diagnosis requires peripheral cytopenia plus at least one of the other criteria, while excluding other causes of low blood counts.
Treatment Options for Myelodysplastic Syndromes (MDS)
Treatment for MDS depends on whether the patient is considered lower-risk or higher-risk, as well as age, overall health, and other medical conditions. The main goals are to improve blood counts, manage symptoms, prevent complications, and, in higher-risk cases, slow disease progression or achieve cure.
Lower-risk MDS (focus on symptom control and quality of life):
- Erythropoiesis-stimulating substances to improve anemia
- Colony-stimulating factors (such as G-CSF or GM-CSF) to support white blood cell production
- Blood transfusions to manage anemia or low platelet counts
- Immunomodulatory substances for patients with specific chromosomal changes (e.g., 5q deletion)
Higher-risk MDS (focus on survival and disease progression):
- Allogeneic hematopoietic stem cell transplantation (from a related or unrelated matched donor) – the only potential cure
- Hypomethylating substances (such as azacitidine or decitabine) to slow progression and improve blood counts
- Supportive care and monitoring for patients without significant symptoms
Key Takeaways
- Myelodysplastic syndromes (MDS) are rare blood cancers that impair healthy blood cell production.
- They mainly affect older adults and can progress to acute myeloid leukemia (AML).
- Diagnosis requires bone marrow evaluation and exclusion of other conditions.
- Treatment strategies differ by risk level: improving blood counts and symptoms in lower-risk patients, and prolonging survival in higher-risk cases.
- Stem cell transplantation remains the only potentially curative treatment.
Sources: